https://www.vascular.abbott/content/dam/bss/divisionalsites/av/products/valve-sizer-isi.pdf
RX ONLY
INDICATIONS FOR USE
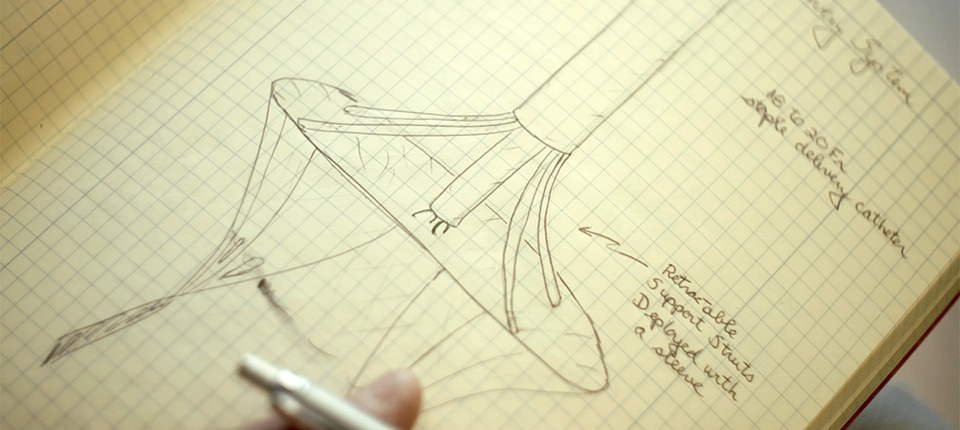
The SJM™ Masters Series Mechanical Heart Valve is intended for use as a replacement valve in patients with a diseased, damaged, or malfunctioning mitral or aortic heart valve. This device may also be used to replace a previously implanted mitral or aortic prosthetic heart valve. The sizer model 905-15 is indicated to confirm size selection of the 15AHPJ-505 and 15MHPJ-505 valves.
CONTRAINDICATIONS
The SJM™ Masters Series Mechanical Heart Valve is contraindicated for individuals unable to tolerate anticoagulation therapy. The sizer model 905-15 is contraindicated for use with any devices other than the 15 AHPJ-505 and 15MHPJ-505 valves. Any sizer sterilization method other than steam is contraindicated.
WARNINGS
Valve
For single use only. Attempts to reuse the valve may result in valve malfunction, inadequate sterilization, or patient harm. Use only St. Jude Medical™ mechanical heart valve sizers.
Do not use if: The valve has been dropped, damaged, or mishandled in any way.
The expiration date has elapsed.
The tamper-evident container seal or inner/ outer tray seals are damaged, broken, or missing.
Remove any residual tissue that may impair valve size selection, correct seating of the valve, rotation of the valve, or leaflet motion.
Proper valve size selection is crucial. Do not oversize the valve. If the native annulus measurement falls between two SJM™ Masters Series Mechanical Heart Valve sizes, use the smaller prosthetic valve size.
The outer tray is not sterile, and should not be placed in the sterile field.
To minimize direct handling of the valve during implantation, do not remove the holder/rotator until the valve has been seated in the annulus.
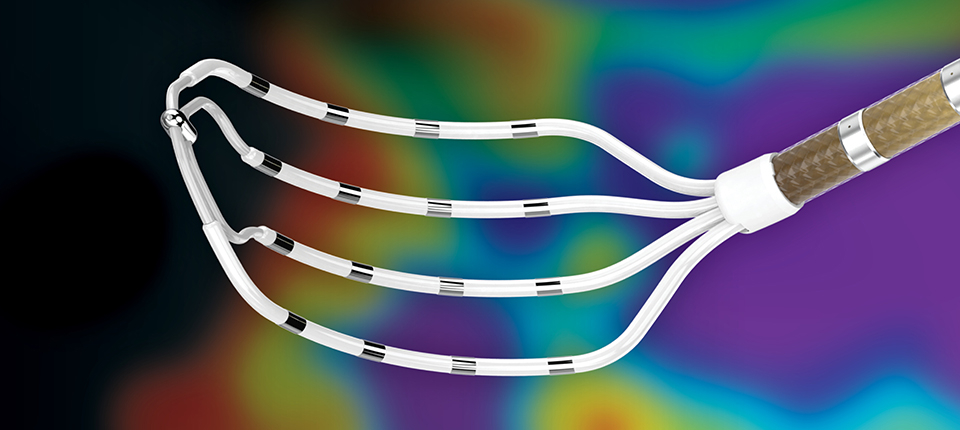
Do not use hard or rigid instruments to test leaflet mobility, as this may result in structural damage to the valve or thromboembolic complications. Use a St. Jude Medical™ leaflet tester to gently test valve leaflet mobility.
Place sutures in the outer half of the valve sewing cuff.
Never apply force to the valve leaflets. Force may cause structural damage to the valve.
Use only SJM™ Valve Holder/Rotators to perform valve rotation. Use of other instruments could result in structural damage. The valve holder/rotator is intended for single use only and should be discarded after surgery.
The two retention sutures on the valve holder/ rotator must be cut and removed before the valve can be rotated.
Do not pass catheters or other instruments through St. Jude Medical™ mechanical heart valves. This could result in scratched or damaged valve components, leaflet fracture, or dislodgment.
Cut suture ends short, especially in the vicinity of the pivot guards, to prevent leaflet impingement
PRECAUTIONS
Valve
Do not touch the prosthetic valve unnecessarily, even with gloved hands. This may cause scratches or surface imperfections that may lead to thrombus formation.
Be careful not to cut or tear the valve sewing cuff when removing the identification tag and the holder/rotator from the valve.
Before placing sutures in the valve sewing cuff, verify that the valve is mounted correctly on the valve holder/rotator.
To avoid structural damage, the valve must be rotated in the fully open position.
To minimize rotational torque, verify that the valve holder/rotator is properly seated in the valve, and that the valve holder handle is perpendicular to the valve.
Remove any loose suture or thread, which may be a source of thrombus or thromboembolism.
Implantation of a prosthetic valve too large for the annulus may result in increased risk of damage to the conductive system, obstruction of the left ventricular outflow tract, impairment of valve mobility, damage to the left circumflex artery, and damage to surrounding tissues or cardiac structures including obstruction and/or distortion of adjacent cardiac structures.
NOTE: PROSPECTIVE DATA TO SUPPORT SAFETY AND EFFECTIVENESS OF THE 15-mm HP VALVE IMPLANTED IN THE AORTIC POSITION ARE NOT CURRENTLY AVAILABLE.
Sizer
Instruments must be cleaned and sterilized prior to use.
Do not use cracked, deformed, discolored/rusted, or damaged instruments.
Improper cleaning may result in an immunological or toxic reaction.
Instrument sterilization temperature must not exceed 280°F (138°C).
Do not bend flexible instrument handles beyond a 90° angle.
Instruments must be sterilized in a tray or container that is permeable to steam.
Do not expose instruments to cleaning or rinse agents that are not compatible with polysulfone or polyphenylsulfone.
POTENTIAL ADVERSE EVENTS
Complications associated with replacement mechanical heart valves include, but are not limited to, hemolysis, infections, thrombus, or thromboembolism, valve dehiscence, unacceptable hemodynamic performance, hemorrhagic complications secondary to anticoagulation therapy, heart block requiring pacemaker implant, prosthetic failure, adjacent cardiac structure interference, heart failure, stroke, myocardial infarction, or death. Any of these complications may require reoperation or explantation of the device.







FOLLOW ABBOTT