Important Safety Information
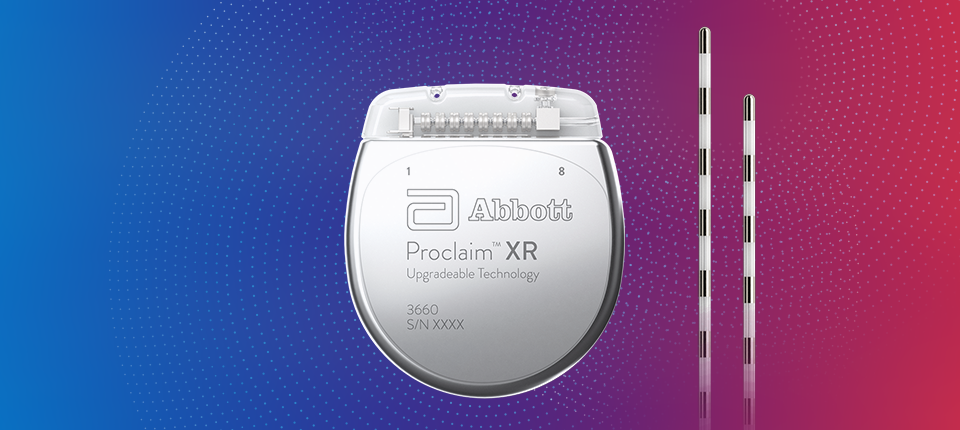
PROCLAIM XR SCS
PRESCRIPTION AND SAFETY INFORMATION
Read this section to gather important prescription and safety information.
INTENDED USE
This neurostimulation system is designed to deliver low-intensity electrical impulses to nerve structures. The system is intended to be used with leads and associated extensions that are compatible with the system.
INDICATIONS FOR USE
This neurostimulation system is indicated as an aid in the management of chronic, intractable pain of the trunk and/or limbs, including unilateral or bilateral pain associated with the following: failed back surgery syndrome and intractable low back and leg pain.
CONTRADICTIONS
This system is contraindicated for patients who are unable to operate the system or who have failed to receive effective pain relief during trial stimulation.
MRI SAFETY INFORMATION
Some models of this system are Magnetic Resonance (MR) Conditional, and patients with these devices may be scanned safely with magnetic resonance imaging (MRI) when the conditions for safe scanning are met. For more information about MR Conditional neurostimulation components and systems, including equipment settings, scanning procedures, and a complete listing of conditionally approved components, refer to the MRI procedures clinician's manual for neurostimulation systems (available online at manuals.sjm.com). For more information about MR Conditional products, visit the Abbott product information page at neuromodulation.abbott.
WARNINGS
The following warnings apply to this neurostimulation system.
Poor surgical risks. Neurostimulation should not be used on patients who are poor surgical risks or patients with multiple illnesses or active general infections.
Magnetic resonance imaging (MRI). Some patients may be implanted with the components that make up a Magnetic Resonance (MR) Conditional system, which allows them to receive an MRI scan if all the requirements for the implanted components and for scanning are met. A physician can help determine if a patient is eligible to receive an MRI scan by following the requirements provided by Abbott Medical. Physicians should also discuss any risks of MRI with patients.
Patients without an MR Conditional neurostimulation system should not be subjected to MRI because the electromagnetic field generated by an MRI may damage the device electronics and induce voltage through the lead that could jolt or shock the patient.
Diathermy therapy. Do not use short-wave diathermy, microwave diathermy, or therapeutic ultrasound diathermy (all now referred to as diathermy) on patients implanted with a neurostimulation system. Energy from diathermy can be transferred through the implanted system and cause tissue damage at the location of the implanted electrodes, resulting in severe injury or death.
Diathermy is further prohibited because it may also damage the neurostimulation system components. This damage could result in loss of therapy, requiring additional surgery for system implantation and replacement. Injury or damage can occur during diathermy treatment whether the neurostimulation system is turned on or off.
Electrosurgery. To avoid harming the patient or damaging the neurostimulation system, do not use monopolar electrosurgery devices on patients with implanted neurostimulation systems. Before using an electrosurgery device, place the device in Surgery Mode using the patient controller app or clinician programmer app. Confirm the neurostimulation system is functioning correctly after the procedure.
During implant procedures, if electrosurgery devices must be used, take the following actions:
Use bipolar electrosurgery only.
- Complete any electrosurgery procedures before connecting the leads or extensions to the neurostimulator.
- Keep the current paths from the electrosurgery device as far from the neurostimulation system as possible.
- Set the electrosurgery device to the lowest possible energy setting.
- Confirm that the neurostimulation system is functioning correctly during the implant procedure and before closing the neurostimulator pocket.
Implanted cardiac systems. Physicians need to be aware of the risk and possible interaction between a neurostimulation system and an implanted cardiac system, such as a pacemaker or defibrillator. Electrical pulses from a neurostimulation system may interact with the sensing operation of an implanted cardiac system, causing the cardiac system to respond inappropriately. To minimize or prevent the implanted cardiac system from sensing the output of the neurostimulation system, (1) maximize the distance between the implanted systems; (2) verify that the neurostimulation system is not interfering with the functions of the implanted cardiac system; and (3) avoid programming either device in a unipolar mode (using the device’s can as an anode) or using neurostimulation system settings that interfere with the function of the implantable cardiac system.
Pediatric use. Safety and effectiveness of neurostimulation for pediatric use have not been established.
Pregnancy and nursing. Safety and effectiveness of neurostimulation for use during pregnancy and nursing have not been established.
Device components. The use of components not approved for use by Abbott Medical with this system may result in damage to the system and increased risk to the patient.
Case damage. Do not handle the IPG if the case is pierced or ruptured because severe burns could result from exposure to battery chemicals.
IPG disposal. Return all explanted IPGs to Abbott Medical for safe disposal. IPGs contain batteries as well as other potentially hazardous materials. Do not crush, puncture, or burn the IPG because explosion or fire may result.
PRECAUTIONS
The following precautions apply to this neurostimulation system.
General Precautions
- Clinician training. Implanting physicians should be experienced in the diagnosis and treatment of chronic pain syndromes and have undergone surgical and device implantation training.
- Patient selection. It is extremely important to select patients appropriately for neurostimulation. Thorough psychiatric screening should be performed. Patients should not be dependent on drugs and should be able to operate the neurostimulation system.
- Infection. Follow proper infection control procedures. Infections related to system implantation might require that the device be explanted.
- Electromagnetic interference (EMI). Some equipment in home, work, medical, and public environments can generate EMI that is strong enough to interfere with the operation of a neurostimulation system or damage system components. Patients should avoid getting too close to these types of EMI sources, which include the following examples: commercial electrical equipment (such as arc welders and induction furnaces), communication equipment (such as microwave transmitters and high-power amateur transmitters), high-voltage power lines, radiofrequency identification (RFID) devices, and some medical procedures (such as therapeutic radiation and electromagnetic lithotripsy).
- Security, antitheft, and radiofrequency identification (RFID) devices. Some antitheft devices, such as those used at entrances or exits of department stores, libraries, and other public places, and airport security screening devices may affect stimulation. Additionally, RFID devices, which are often used to read identification badges, as well as some tag deactivation devices, such as those used at payment counters at stores and loan desks at libraries, may also affect stimulation. Patients who are implanted with nonadjacent multiple leads and patients who are sensitive to low stimulation thresholds may experience a momentary increase in their perceived stimulation, which some patients have described as uncomfortable or jolting. Patients should cautiously approach such devices and should request help to bypass them. If they must go through a gate or doorway containing this type of device, patients should turn off their IPG and proceed with caution, being sure to move through the device quickly.
- Wireless use restrictions. In some environments, the use of wireless functions (e.g., Bluetooth® wireless technology) may be restricted. Such restrictions may apply aboard airplanes, in hospitals, near explosives, or in hazardous locations. If you are unsure of the policy that applies to the use of this device, please ask for authorization to use it before turning it on. (Bluetooth® is a registered trademark of Bluetooth SIG, Inc.)
- Mobile phones. While interference with mobile phones is not anticipated, technology continues to change and interaction between a neurostimulation system and a mobile phone is possible. Advise patients to contact their physician if they are concerned about their mobile phone interacting with their neurostimulation system.
Sterilization and Storage
- Single-use, sterile device. The implanted components of this neurostimulation system are intended for a single use only. Sterile components in this kit have been sterilized using ethylene oxide (EtO) gas before shipment and are supplied in sterile packaging to permit direct introduction into the sterile field. Do not resterilize or reimplant an explanted system for any reason.
- Storage environment. Store components and their packaging where they will not come in contact with liquids of any kind.
Handling and Implantation
- Expiration date. An expiration date (or “use-before” date) is printed on the packaging. Do not use the system if the use-before date has expired.
- Care and handling of components. Use extreme care when handling system components prior to implantation. Excessive heat, excessive traction, excessive bending, excessive twisting, or the use of sharp instruments may damage and cause failure of the components.
- Package or component damage. Do not implant a device if the sterile package or components show signs of damage, if the sterile seal is ruptured, or if contamination is suspected for any reason. Return any suspect components to Abbott Medical for evaluation.
- System testing. To ensure correct operation, always test the system during the implant procedure, before closing the neurostimulator pocket, and before the patient leaves the surgery suite explanted.
- Device modification. The equipment is not serviceable by the customer. To prevent injury or damage to the system, do not modify the equipment. If needed, return the equipment to Abbott Medical for service.
Hospitals and Medical Environments
- High-output ultrasonics and lithotripsy. The use of high-output devices, such as an electrohydraulic lithotriptor, may cause damage to the electronic circuitry of an implanted IPG. If lithotripsy must be used, do not focus the energy near the IPG.
- Ultrasonic scanning equipment. The use of ultrasonic scanning equipment may cause mechanical damage to an implanted neurostimulation system if used directly over the implanted system.
- External defibrillators. The safety of discharge of an external defibrillator on patients with implanted neurostimulation systems has not been established.
- Therapeutic radiation. Therapeutic radiation may damage the electronic circuitry of an implanted neurostimulation system, although no testing has been done and no definite information on radiation effects is available. Sources of therapeutic radiation include therapeutic X rays, cobalt machines, and linear accelerators. If radiation therapy is required, the area over the implanted IPG should be shielded with lead. Damage to the system may not be immediately detectable.
ADVERSE EFFECTS
In addition to those risks commonly associated with surgery, the following risks are associated with implanting or using this IPG:
- Unpleasant sensations or motor disturbances, including involuntary movement, caused by stimulation at high outputs (If either occurs, turn off your IPG immediately.)
- Stimulation in unwanted places (such as radicular stimulation of the chest wall)
- Paralysis, weakness, clumsiness, numbness, or pain below the level of the implant
- Persistent pain at the electrode or IPG site
- Seroma (mass or swelling) at the IPG site
- Allergic or rejection response to implant materials
- Implant migration or skin erosion around the implant
- Battery failure